Discussion
Discussion
Soliris (eculizumab) for atypical hemolytic uremic syndrome
Last updated June 21, 2024, by Marisa Wexler, MS

What is Soliris for aHUS?
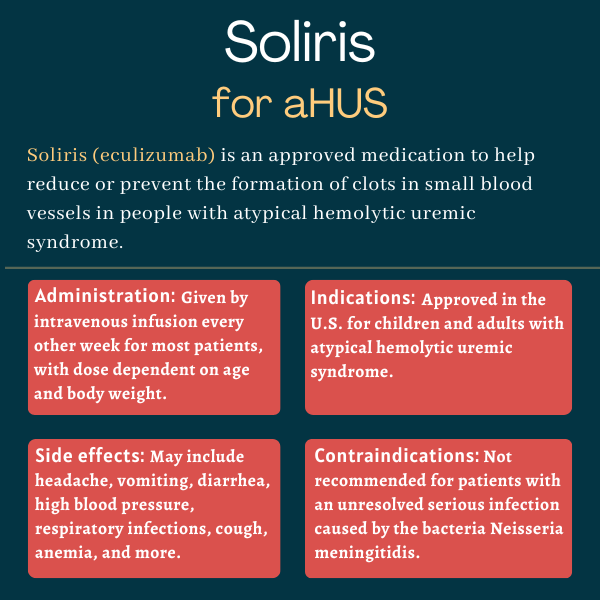
Soliris (eculizumab) is a monoclonal antibody that’s approved for patients with atypical hemolytic uremic syndrome (aHUS). It specifically works to reduce or prevent the formation of clots in small blood vessels throughout the body, a consequence of aHUS that drives organ damage.
Soliris, which is administered via an into-the-vein (intravenous) infusion, was originally developed by Alexion Pharmaceuticals, which was acquired in 2021 by AstraZeneca.
It has also been approved by the U.S. Food and Drug Administration (FDA) for myasthenia gravis, paroxysmal nocturnal hemoglobinuria, and neuromyelitis optica spectrum disorder.
Some Soliris biosimilars are also available. Biosimilars are products that contain a version of the same active ingredient that’s functionally equivalent to the name-brand medicine. Bkemv (eculizumab-aeeb), the first interchangeable biosimilar of Soliris to become available in the U.S., was approved in 2024 by the FDA for aHUS and paroxysmal nocturnal hemoglobinuria. It is marketed by Amgen.
Therapy snapshot
| Brand name: | Soliris |
| Chemical name: | Eculizumab |
| Usage: | Reduce or prevent the formation of clots in small blood vessels |
| Administration: | Intravenous infusion |
How does Soliris work?
The complement cascade is a part of the immune system that normally helps the body fend off infections. aHUS is a rare disorder in which mutations in complement regulator genes, such as CFH, MCP (CD46), and CFI, result in the uncontrolled activation of part of the complement cascade called the alternative complement pathway. This, in turn, leads to thrombotic microangiopathy (TMA), a condition in which clots form in small blood vessels throughout the body, damaging organs.
In the alternative complement pathway, a complement protein called C5 is cleaved into two forms, called C5a and C5b, by the enzyme C5 convertase. While C5a is a proinflammatory molecule, C5b combines with other proteins to form the C5b-9 terminal membrane attack complex. C5b-9 is known to promote clotting within blood vessels via the aggregation, or bringing together, of platelets.
Soliris is a humanized monoclonal antibody that binds to C5 and prevents its cleavage into C5a and C5b. This prevents the formation of the terminal complement complex C5b-9 and stops clotting within small blood vessels.
Who with aHUS can take Soliris?
The FDA approved Soliris to inhibit complement-mediated TMA in children and adults with aHUS in September 2011. In the same year, the European Commission granted marketing authorization for Soliris to treat children and adults with aHUS.
Because Soliris increases the risk of serious meningococcal infections, it is available in the U.S. only through a restricted program called Ultomiris and Soliris REMS. REMS stands for Risk Evaluation and Mitigation Strategy. Healthcare providers must enroll in the REMS program and get special certification to prescribe Soliris. Additionally, prescribers must inform patients of the potential risks of treatment and assess their vaccination status for meningococcal vaccines, ensuring they meet current recommendations before receiving treatment. The program also ensures that only certified pharmacies can dispense the medication.
Who should not take Soliris?
Soliris is contraindicated, or not recommended, for people who have an unresolved serious infection with the bacteria Neisseria meningitidis, which can cause meningitis and other forms of meningococcal disease.
The prescribing label for Soliris has a boxed warning for serious, life-threatening meningococcal infections, as these have been reported in patients treated with complement inhibitors. Meningococcal infections can rapidly become life-threatening or fatal if not identified and treated early. Patients should be carefully monitored for signs of infection.
The boxed warning also notes that patients should complete or update their vaccinations against meningococcal infections before starting treatment with Soliris, unless the benefits of treatment clearly outweigh the risk of a serious infection.
Also of note, while Soliris is approved for aHUS, it is not indicated for “typical” HUS, also called STEC-HUS, which is a disorder caused by toxins produced by certain bacteria, most commonly Escherichia coli.
How is Soliris administered in aHUS?
Soliris is available in single-use vials that contain 300 mg of the medication in 30 mL of a clear, colorless liquid.
The therapy is administered via an infusion into the bloodstream. In aHUS patients 18 and older, each infusion takes a bit longer than half an hour, and the recommended dosing schedule is:
- 900 mg weekly for the first four weeks
- 1,200 mg in the fifth week
- 1,200 mg every other week thereafter.
In children and adolescents with aHUS who are younger than 18, Soliris infusions last one to four hours and are dosed according to the individual’s body weight:
- Pediatric patients who weigh 40 kg (88 pounds) or more are treated with the same dosing schedule as the one for adults.
- Pediatric patients weighing 30 kg (66 pounds) to less than 40 kg, are given 600 mg weekly for two weeks, then 900 mg in the third week, and 900 mg every other week thereafter.
- Pediatric patients weighing 20 kg (44 pounds) to less than 30 kg are given 600 mg weekly for two weeks, then 600 mg in the third week, and 600 mg every other week thereafter.
- Pediatric patients weighing 10 kg (22 pounds) to less than 20 kg are given 600 mg in the first week, 300 mg in the second week, and 300 mg every other week thereafter.
- Pediatric patients weighing 5 kg (11 pounds) to less than 10 kg are given 300 mg in the first and second week of treatment, then 300 mg every three weeks thereafter.
Patients of all ages should be monitored for infusion reactions during the infusion itself and for at least one hour afterward. If an infusion reaction occurs, the infusion may be slowed or stopped at the discretion of a doctor.
If someone with aHUS who has been on Soliris needs to stop taking it, the patient should be monitored for signs of recurring TMA, such as altered mental state, seizures, shortness of breath, or chest pain, for at least 12 weeks after stopping Soliris. If TMA complications occur after stopping treatment, physicians may consider starting patients on Soliris again, resort to plasma therapy, or other appropriate organ-specific supportive measures.
Treatment with Soliris should not alter anticoagulant (anti-clotting) management.
Soliris in clinical trials
The safety and efficacy of Soliris for the treatment of aHUS was evaluated in five clinical studies. In all of them, Soliris was given to adults and adolescents following the currently recommended dosing schedule: a 900 mg dose every week for four weeks, followed by a fifth dose of 1,200 mg a week later, and then 1,200 mg every other week thereafter. The dosing schedule for children weighing less than 40 kg was based on body weight.
C08-002A/B and C08-003A/B trials
One of the studies, a Phase 2 trial called C08-002A/B (NCT00844545 and NCT00844844), tested Soliris in 17 people with aHUS who continued showing signs of TMA despite plasma exchange — a treatment that involves replacing plasma, the liquid portion of blood — or infusion. The trial’s main goal was to see if treatment with Soliris would lead to an increase in the levels of platelets, which are cell fragments involved in blood clotting. In patients experiencing TMA, platelet counts tend to dip due to abnormal blood clotting.
A similar Phase 2 study, called C08-003A/B (NCT00838513 and NCT00844428), tested Soliris in 20 people with aHUS who were responding to plasma exchange or infusion and generally had no signs of TMA while on chronic plasma treatment. In that study, the main goal was to evaluate how many patients were TMA-free, defined as having steady platelet counts without needing additional plasma exchange or infusion or requiring kidney dialysis, for at least 12 weeks.
In both studies, patients received Soliris for at least 26 weeks, or about six months.
Results showed both Phase 2 studies met their main goals: in C08-002A/B, patients’ platelet levels increased by more than 70 billion platelets per liter of blood after six months, and in C08-003A/B, 16 of the 20 patients were TMA-free after six months on Soliris.
In both studies, the majority of patients on Soliris achieved hematologic normalization, which is defined as having steady normal levels of platelets and lactate dehydrogenase (LDH), a marker of cell and tissue injury, for at least four weeks. Improvements in kidney function were also seen. All these benefits were maintained through to two years in both studies.
C10-004 trial
A third Phase 2 study, called C10-004 (NCT01194973), evaluated Soliris in 41 adults with aHUS who showed signs of active TMA. Its main goal was to determine how many patients achieved a complete TMA response, defined as normalization in the levels of platelets and LDH, alongside a reduction of at least 25% in a marker of kidney dysfunction called creatinine for at least four weeks.
As in the previous studies, patients participating in this trial received treatment with Soliris for at least 26 weeks.
Results showed most patients achieved a TMA response, with nearly 90% attaining hematologic normalization. Kidney function also improved.
C10-003 trial
A fourth Phase 2 trial, C10-003 (NCT01193348), tested Soliris in 22 children with aHUS, as young as a few months old. Similar to the C10-004 trial in adults, the main goal of this study was to assess the proportion of patients achieving a complete TMA response. Patients participating in C10-003 also received treatment with Soliris for at least 26 weeks.
After six months on the therapy, 14 (64%) achieved a complete TMA response, with most showing hematologic normalization and improvements in kidney function.
C09-001r study
The fifth study, called C09-001r (NCT01770951), was a retrospective review of aHUS patients who had received Soliris outside of Alexion-sponsored trials.
Data from 19 patients in the study showed outcomes were generally consistent with findings from the other trials, with 42% of patients achieving a complete TMA response and most showing normalization of platelet counts.
Common side effects of Soliris
The most common side effects of Soliris seen in clinical trials of aHUS patients include:
- headache
- diarrhea
- vomiting and nausea
- high blood pressure (hypertension)
- upper respiratory infection or the common cold (nasopharyngitis)
- cough
- anemia
- urinary tract infections
- abdominal pain
- fever
- swelling of the extremities.
Serious meningococcal infections
Soliris carries a boxed warning noting it can increase the risk of meningococcal infections, a type of bacterial infection that can be life-threatening and has been observed in both vaccinated and unvaccinated patients treated with complement inhibitors. The therapy is contraindicated in patients who have a serious unresolved infection caused by the bacteria Neisseria meningitidis, and it should be used with care in people who have other types of systemic infections.
Except in extenuating circumstances where immediate treatment is crucial, patients should receive vaccination against meningococcal bacteria (serogroups A, C, W, Y, and B) at least two weeks before starting treatment with Soliris. If circumstances require treatment be started in patients who aren’t yet vaccinated, preventive antibiotic therapy should be given and vaccines should be administered as soon as possible. Providers prescribing Soliris should follow the most updated guidelines for meningococcal vaccination from the Advisory Committee on Immunization Practices (ACIP), noting these guidelines include specific recommendations for patients on complement-blocking therapies like Soliris.
Vaccination reduces the risk of infection, but doesn’t completely eliminate it. Therefore, it’s possible for meningococcal infections to occur even in patients who have been vaccinated. As such, patients taking Soliris should be closely monitored for these infections, and informed of the signs and symptoms, seeking immediate medical care if these occur. If an infection is suspected, patients should be immediately evaluated and promptly treated.
If a serious infection develops, treatment with Soliris may be interrupted.
Other infections
Serious infections caused by other Neisseria species, including disseminated gonococcal infections, have also been reported.
Patients treated with Soliris may be more susceptible to developing infections, particularly those caused by encapsulated bacteria, such as Streptococcus pneumoniae and Haemophilus influenzae, due to the therapy’s mechanism of action. Children treated with Soliris may also be at higher risk of developing serious infections caused by S. pneumoniae and H. influenzae type b. Vaccination to prevent infections caused by these bacteria should be administered according to ACIP recommendations.
Infusion-related reactions
Reactions occurring during or shortly after a Soliris infusion, including allergic reactions, have been reported. Patients should be monitored for such reactions during each infusion. If a serious reaction occurs, including cardiovascular instability or respiratory compromise, the treatment should be stopped and appropriate supportive therapies given.
Use in pregnancy and breastfeeding
Data on the use of Soliris during pregnancy is limited. An analysis of more than 300 pregnant women who were exposed to Soliris during pregnancy did not detect any major safety concerns, but since the sample size was fairly small, it’s impossible to say definitively whether or not Soliris is safe to use during pregnancy. Animal studies, however, showed that a similar compound (an anti-C5 antibody) could cause harm to a developing fetus. Untreated aHUS can also increase the risk of poor outcomes for both the mother and the fetus, so the benefits and risks of using Soliris during pregnancy should be carefully weighed.
It is also not clear if Soliris can pass into breast milk or whether its use while breastfeeding may be harmful for the nursing infant. As with pregnancy, the potential risks and benefits of using Soliris while breastfeeding need to be carefully considered on a case-by-case basis.
aHUS News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- My community helps me navigate the ultra-rare reality of living with aHUS
- Dual therapy manages aHUS with high blood pressure: Case report
- Caregivers are the unsung heroes of the rare disease world
- aHUS drug Soliris helps reverse organ failure in young woman in rare case
- A ‘glow-up’ is just the boost I’ve needed in life with rare diseases
- Unexpected gene therapy finding may help treat two rare kidney diseases
- How aHUS treatment led to my first tattoos
- Ultomiris at lower doses just as safe, effective for children with aHUS: Study
- Strange symptoms make me wonder if I’m having neurological complications
- Leaky artificial heart valve triggers rare aHUS in woman, 70: Report
Related articles
-
 Discussion
Discussion