Severe Hypertension Common in aHUS Patients and Soliris Effective at Treating Them, Study Finds
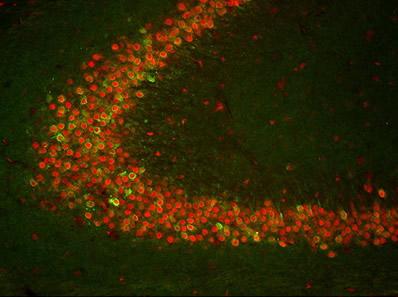
"TIA-1 is known for its ability to regulate gene expression during cellular stress,"James Hewett, associate professor of biology, said in a press release. "We suspected that TIA-1 was involved with seizure suppression, but our findings suggested something else." Credit: Courtesy of Elsevier
Severe and life-threatening hypertension is common in people with atypical hemolytic uremic syndrome (aHUS), and Soliris (eculizumab) is a more effective than plasmapheresis in treating these patients, a Spanish study finds.
The study, “Severe and malignant hypertension are common in primary atypical hemolytic uremic syndrome,” was published in the journal Kidney International.
aHUS belongs to a group of rare disorders called thrombotic microangiopathies (TMAs), which are characterized by the presence of hemolytic anemia (destruction of red blood cells), low levels of platelets, and the formation of blood clots in small blood vessels that lead to organ damage.
aHUS results from an abnormal activation of the complement system (a set of more than 50 blood proteins that contribute to the body’s natural immune defenses) that is estimated to be caused by mutations in the complement system in roughly 60% of patients.
Malignant hypertension — a rapidly increase in blood pressure causing sudden and severe damage to the brain, eyes, and kidneys — has been considered a cause of secondary TMA, mostly due to damage to small blood vessels in those organs through the extreme increase in pressure.
“However, if an extreme increase of [blood pressure], secondary to well-identified diseases, can by itself induce a TMA, it has not been analyzed in large [group] of patients,” the researchers wrote.
Recent reports of mutations in complement genes in people with hypertension-induced TMA raise the possibility that these patients may instead have aHUS with severe and malignant hypertension.
The distinction between these two conditions is critical for a rapid initiation of appropriate treatment, which in the case of aHUS would be Soliris. Soliris, by Alexion, works by blocking the uncontrolled hyperactivity of the complement system.
However, the frequency and severity of hypertension in aHUS patients is largely unknown, and data is limited on the effectiveness of Soliris in aHUS patients with severe and malignant hypertension.
To fill this gap, researchers in Spain, in collaboration with the Spanish Group for the Study of Glomerular Diseases (GLOSEN), evaluated the frequency and severity of hypertension in 55 people with aHUS, and whether Soliris treatment was effective in those with severe and malignant hypertension.
They analyzed the patients’ clinical data, the presence of mutations in complement genes, and the occurrence of malignant hypertension in those with severe (grade 2 or 3) hypertension through funduscopic examination — an eye exam that can detect damage to blood vessels of the retina and swelling of the optic nerve.
Mean age of the participants (45 Caucasians, five Hispanics, three Africans, and two Asians) was 34 years, and 33 of them (60%) were women.
A total of 36 patients (65%) had severe hypertension, and 19 of them (53%) had the malignant form (16 with grade 3 and three with grade 2 hypertension).
Patients with severe hypertension had significantly worse kidney function than those with mild hypertension (grade 1), but no significant differences were found between patients with or without malignant hypertension, except for blood pressure.
Disease-causative mutations in genes of the complement system were detected in 19 patients (53%), seven with malignant hypertension. There were no significant differences between patients with or without disease-causative mutations or in their proportions across the different groups of hypertension.
A total of 46 people received plasmapheresis and 26 were given Soliris, and Soliris induced significantly more blood and kidney responses (81%) than plasmapheresis (24%) in these patients. Soliris benefits were also observed in patients with malignant hypertension, and regardless of the presence of mutations in complement genes.
In patients without complement mutations, Soliris was stopped after a median of six months and no relapses were detected.
Researchers also compared the clinical features and the frequency of TMA between the 55 aHUS patients and 110 people with malignant hypertension caused by other diseases.
They found that while people with malignant hypertension but not aHUS showed significantly higher blood pressure than aHUS patients, only six of them (5%) had TMA. This suggested that an extreme increase in blood pressure does not induce TMA by itself.
People with malignant hypertension due to other diseases also had significantly less severe acute kidney injury and were older than those with aHUS.
These data highlight that severe and life-threatening hypertension is common in aHUS patients, while TMA is rare in people with malignant hypertension associated with other diseases.
Based on these findings, “complement dysregulation should be suspected in patients with severe or malignant [hypertension] accompanied by TMA,” especially in “young patients with a severe [acute kidney injury], without apparent causes of hypertension and with [kidney] function that does not improve despite [blood pressure] control,” the researchers wrote.






