Soliris may induce remission of aHUS in children with anti-FH antibodies
Observed results occurred despite type of immunosuppressive used
Soliris (eculizumab) can effectively induce and maintain remission of atypical hemolytic uremic syndrome (aHUS) in children with autoantibodies that target complement factor H (FH).
That’s according to a study that found the therapy reduced anti-FH antibodies no matter the type of immunosuppressive treatments used with it. They also lowered in patients who were only treated with Soliris.
“Taken together, our results suggest that a strategy associating eculizumab with [mycophenolate mofetil] monotherapy could be sufficient in some anti-FH antibody-associated HUS cases and that [plasma exchange] may be avoided in most patients,” the researchers wrote in “Anti-CFH-associated hemolytic uremic syndrome: do we still need plasma exchange?,” which was published in Pediatric Nephrology.
aHUS is a type of thrombotic microangiopathy, a group of diseases marked by red blood cell destruction, or hemolytic anemia, low platelet counts, and blood clots in small vessels that can cause organ damage, particularly to the kidneys.
Most people with aHUS have predisposing genetic mutations that cause a part of the immune system called the complement cascade to become overactive. The disease is caused by autoantibodies against a complement protein called factor H, or FH, in between 5-50% of children with aHUS.
The main therapeutic strategies for such cases include plasma exchange therapy to remove the autoantibodies circulating in the bloodstream and medications to suppress the immune system, including steroids, mycophenolate mofetil (MMF), and/or rituximab.
Soliris with immunosuppressive therapies
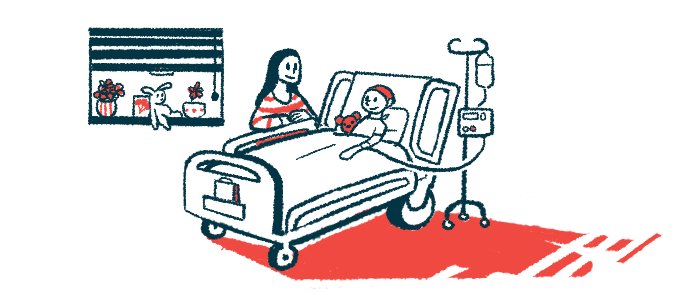
Recently, combining Soliris with immunosuppressive therapies has been proposed to induce remission of aHUS. Here, researchers retrospectively studied 12 children (eight boys) with aHUS caused by anti-FH antibodies who were treated with Soliris and immunosuppressive medications at four medical centers in Italy and France to help “determine the optimal treatment protocol” in aHUS. The children’s ages were between 5 months and 17 years, and they were followed for a median of 49 months, or about four years.
All had signs of hemolytic anemia and thrombocytopenia, or low platelet counts. Also, they all had impaired kidney function and acute kidney injury, as assessed by the presence of proteins in the urine and a low estimated glomerular filtration rate (eGFR). Two children required dialysis.
Three had signs of liver inflammation, or hepatitis, and one had neurological and cardiac involvement. Another patient had diabetes. Ten children had genetic mutations in the factor H-related genes CFHR1 and CFHR3, a known cause of aHUS.
Induction treatment included Soliris in 10 children. Three patients were treated with plasma exchange or IgG adsorption, which removes antibodies from the bloodstream. Two of the three were also on Soliris.
Three patients were given MMF alone, one MMF and steroids, one MMF and rituximab, and three received MMF or steroids along with rituximab. Four patients didn’t receive immunosuppressive therapies.
The median time to disease remission after treatment started was 56 days for blood disease parameters to normalize and 26 days for kidney function to normalize. These periods were shorter for those treated with Soliris, with blood-related parameters taking 42 to normalize and kidney function taking 14 days. At the last follow-up, all but one patient had eGFR levels within the normal range, above 90 mL/min/1.73 m2.
Anti-FH antibody levels in the bloodstream decreased in all but one patient, by 54% after three months of treatment, by 58% after nine months, and by 74% after a year. No difference in antibody levels was observed based on the immunosuppressive treatment used.
Soliris was discontinued in seven patients after a median of 11 months. MMF was stopped in six of the eight patients who received the therapy after three years. None of these patients relapsed and eGFR at the last follow-up was above 70 mL/min/1.73 m2 in all patients, which is close to normal.
Soliris “is effective and safe in inducing and maintaining remission in aHUS secondary to anti-FH antibodies and renders anti-FH [level] reduction less urgent,” the researchers wrote.