Rare Eye Manifestations Linked to aHUS, Study Reports
Written by |
A rare case of a 20-year-old male with atypical hemolytic uremic syndrome (aHUS) showing damage to both eyes that culminated in impaired vision highlights the importance of prompt diagnosis and treatment to ensure better outcomes, a report says.
The study, “Bilateral proliferative retinopathy and ischemic optic neuropathy in a patient with atypical hemolytic-uremic syndrome,” was published in the journal Medicine.
In aHUS, the complement system, a family of proteins found in circulation that helps with the immune response, is overactive and leads to the formation of blood clots in small blood vessels.
This causes problems in two major organs, the heart and kidneys. Eye involvement has rarely been reported in aHUS.
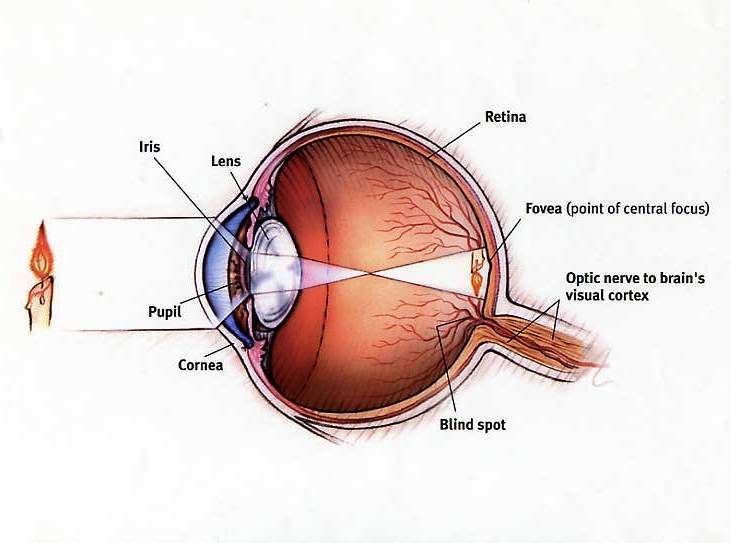
Here, researchers in Taiwan reported the case of the aHUS patient who presented with vitreous hemorrhage — bleeding into the eye’s vitreous humor (the transparent gelatinous tissue filling the eyeball behind the lens) — and tractional retinal detachment (TRD), when the retina is pulled away from the back of the eye, causing immediate vision loss in both eyes.
“To our knowledge, this is the first reported case of atypical HUS complicated by bilateral TRD,” they stated.
Upon admission to the hospital, he had fever, seizures, and altered consciousness. The medical team diagnosed an acute kidney injury and central nervous complications associated with aHUS.
He was given plasma exchange (PEX) each day for two weeks and daily red blood cell transfusions for eight days. Additionally, the patient underwent hemodialysis for one week, and treatment with Ultomiris (ravulizumab, sold by Alexion) for two months. Both renal and neurological symptoms improved over time.
However, within two months, the patient experienced vision deterioration in both eyes. His visual acuity was limited to hand motion at 30 cm for left and right sides.
Eye examination, namely with the dilated eye exam that allows access to the retina and optic nerve, revealed that there was blood inside the retina. This was accompanied by new blood vessel formation in both eyes.
Despite treatment with Ultomiris, the condition did not improve and the patient developed TDR.
At this point, he underwent surgery to fix the retina displacement. Although the retina was well-attached post-surgery, visual acuity did not show improvement.
The team believes that the restrictive blood supply in the retina caused by the abnormal blood clots formed in aHUS caused hypoxia (insufficient oxygen levels) that in turn promoted the release of signals inducing blood vessel formation, but the outcome was weaker vessels that are more prone to damage.
This case highlights the need for physicians to “keep eye involvement and ocular symptoms in mind when examining a patient with aHUS,” the researchers stated.
“Early treatment is essential to avoid vision-threatening complications,” the study concluded.




