Hypertensive Emergency, Complement Mutations Key to aHUS Prognosis, Study Says
Hypertensive emergency and the presence of rare complement mutations are essential to estimate the prognosis of kidney disease in patients with atypical hemolytic uremic syndrome (aHUS).
The study, “Impact Of Hypertensive Emergency And Complement Rare Variants On Presentation And Outcome Of Atypical Hemolytic Uremic Syndrome,” was published in Haematologica.
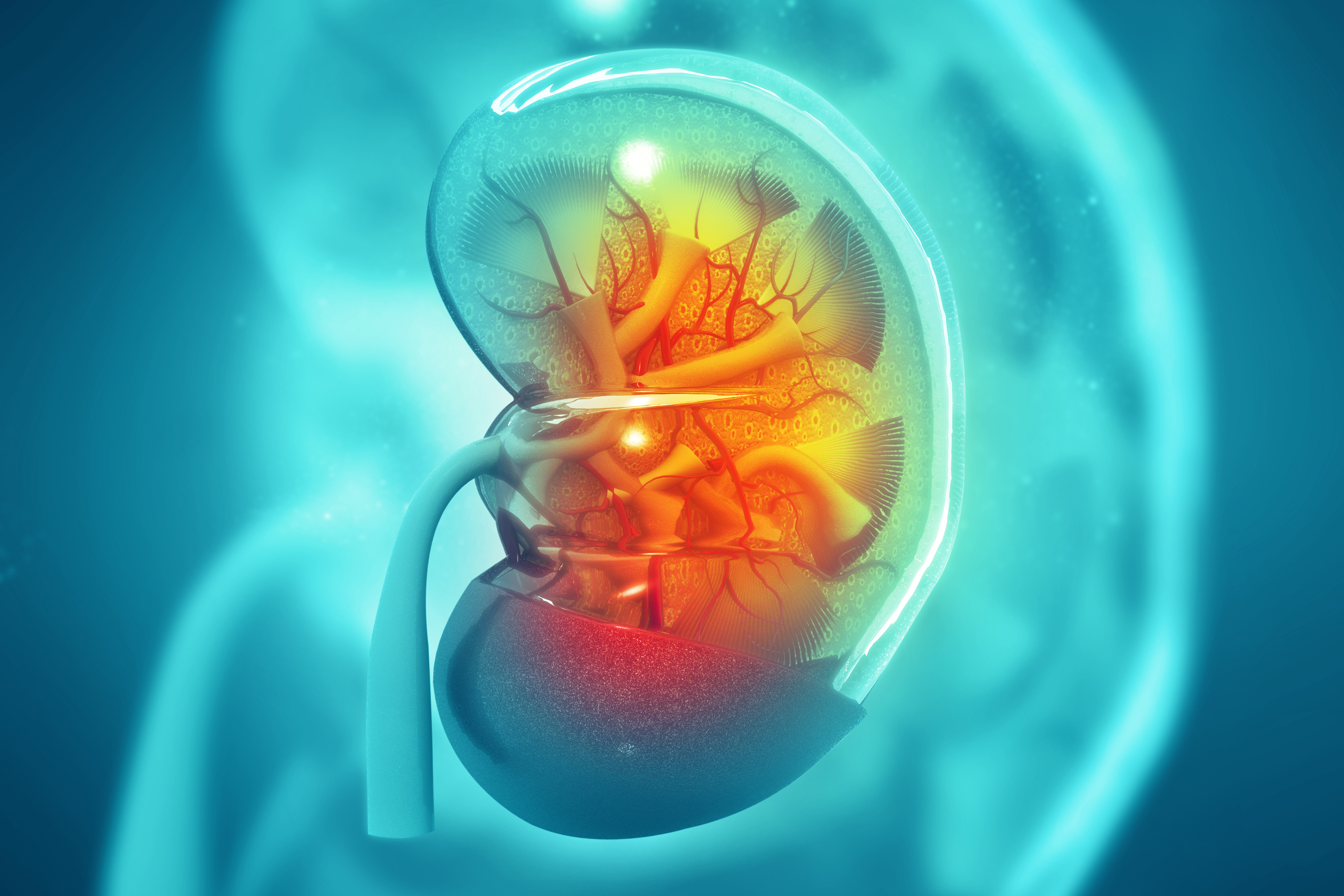
aHUS is caused by the progressive destruction of red blood cells because of a malfunction of the complement system — a set of more than 50 blood proteins that form part of the body’s immune defenses. Damaged red blood cells can aggregate and form clots that clog the kidney’s filtering system, potentially leading to kidney failure.
High blood pressure is one of the most severe complications of aHUS. Recently, some studies have proposed a new medical term known as hypertensive emergency (HE) to describe a condition characterized by high blood pressure and end-organ damage.
“[The similarity between HE and aHUS complications] raises the issue of whether primitive aHUS is complicated by secondary HE, or primary HE leads to secondary aHUS,” the researchers said.
In this study, a group of scientists from French institutions set out to evaluate the clinical, biological, and genetic characteristics of a large group of aHUS patients with and without HE.
The retrospective study involved 76 patients with aHUS and HE (HE-aHUS group) and 61 patients with aHUS without HE (noHE-aHUS group).
Patients from the HE-aHUS group were predominantly men (58%), mean age 37, and a mean systolic/diastolic blood pressure of 214/128 mmHg. About 120/80mmHg and up to 139/89mmHg are considered normal blood pressure values.
In the noHE-aHUS group, fewer than a third of the patients were men (28%), with a mean age of 36 and a mean systolic/diastolic blood pressure of 154/90 mmHg.
Patients with aHUS and HE had slightly higher levels of hemoglobin (8.5 g/dL) compared to those who did not have HE (7.5 g/dL) and were more likely to have neurological impairments.
Genetic analyses identified at least one rare complement mutation in 51.3% and 67% of the patients in the HE-aHUS and noHE-aHUS groups, respectively.
Kidney disease prognosis was severe in both groups, with 23% and 40% of the patients estimated to reach the final stage of kidney disease within five years (five-year renal survival) in the HE-aHUS and noHE-aHUS groups, respectively.
While patients who did not carry complement mutations and did not have HE had a five-year renal survival of 77%, those who had HE and/or complement mutations had less than a 25% chance of reaching the same outcome.
Among those without HE, all patients who had been treated with Soliris (eculizumab) — a complement inhibitor developed and marketed by Alexion — reached five-year renal survival, while 40% of those who were not treated with Soliris attained the same outcome. Conversely, no significant prognosis improvement was found between patients with HE who had been treated with Soliris and those who had not (46% vs 23%, respectively).
“For the first time, we identified HE at onset as a new clinical factor which could associate with long-term prognosis. The renal prognosis was dramatically better in patients without HE nor C variants than all other groups, even in the absence of eculizumab treatment,” the researchers stated.
“HE and genetics allow individualizing patients with highly different renal prognosis and suggest new [disease development] pathways involved in aHUS,” they concluded.