Blindness in one eye is aHUS sign in man, case study reports
30-year-old treated with plasma therapy as Soliris unavailable
Written by |
Physicians in India described the case of atypical hemolytic uremic syndrome (aHUS) that manifested as loss of vision in one eye in a 30-year-old man.
The patient was successfully managed with plasma therapy, because Soliris (eculizumab) was not available.
“This is the first described case to our knowledge of [aHUS] presenting with unilateral blindness,” the authors wrote. The report, “A Unique Presentation of Atypical Hemolytic Uremic Syndrome With Unilateral Blindness and Ischemic Stroke: A Case Report,” was published in Cureus.
aHUS is a form of thrombotic microangiopathy (TMA), a group of disorders characterized by the formation of blood clots in small blood vessels that damage internal organs, particularly the kidneys. These clots arise as a result of the abnormal activation of the complement cascade, a component of the immune system that typically helps defend the body against infections.
Other hallmark features of the disease include low platelet counts (thrombocytopenia) and red blood cell destruction (hemolytic anemia). Some patients with aHUS develop extra-renal, or outside-the-kidney, manifestations that involve the central nervous system (brain and spinal cord), which could present as seizures, stroke, and coma.
Fever, chills accompany blindness in one eye
In the case report, physicians in India wrote about a man whose main manifestation was blindness in one eye.
The man came to the hospital with prolonged fever, accompanied by chills, diarrhea, and blood in the urine. He had experienced progressive vision loss in his left eye over two months, and also had high blood pressure, pallor, and mild yellow skin discoloration.
Lab tests revealed he had anemia, or a low number of red blood cells circulating in the bloodstream. He also had an elevated number of white blood cells (a type of immune cell) and showed signs of kidney dysfunction.
Doctors suspected a generalized bacterial infection and treated him with broad-spectrum antibiotics. But after three days in the hospital, he began bleeding from the rectum.
Additional tests examining the inside of the gastrointestinal tract showed erosions or sores in the lining of the ileum, which is the final portion of the small intestine. Blood tests showed signs of hemolysis, or red blood cell destruction. “Considering a high suspicion” of TMA, the researchers wrote, doctors treated him with six units of fresh frozen plasma and packed red blood cell transfusions.
The patient also developed neurological symptoms, including weakness on one side of the body and changes in awareness and perception. A brain MRI scan revealed damage in several areas of the brain.
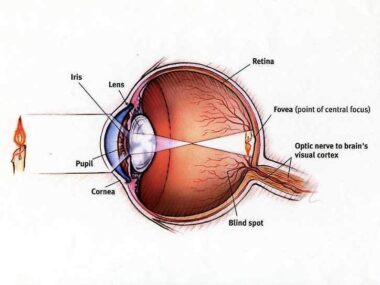
By day six, the patient had complete vision loss in the left eye. His retina, the light-sensitive tissue at the back of the eye, had been damaged due to high blood pressure.
The patient tested negative for self-targeting antibodies, but a kidney biopsy showed alterations that were consistent with TMA. Overall, these observations supported the diagnosis of aHUS. The patient’s family history of kidney failure supported a possible hereditary predisposition to aHUS, further backing the diagnosis.
Because Soliris was not available, treatment focused mainly on plasma therapy. Plasma is the liquid portion of blood that contains water, salts, and proteins, such as antibodies. Providing plasma from healthy donors to aHUS patients may help normalize complement function by supplying functional complement regulatory proteins.
The patient’s kidney function improved, and after 15 days in the intensive care unit, he was discharged.
“Plasma therapy is still the first-line treatment of such patients where [Soliris] is unavailable,” the researchers wrote.