Study Links ADAMTS13 Activity to Improved PEX Treatment Outcomes in aHUS Patients
The activity of a molecule called ADAMTS13 can predict the outcome of patients with with atypical hemolytic uremic syndrome (aHUS) and their response to plasma exchange therapy (PEX), as well as guide treatment decisions, a Korean study suggests.
The study, “Prognostic utility of ADAMTS13 activity for the atypical hemolytic uremic syndrome (aHUS) and comparison of complement serology between aHUS and thrombotic thrombocytopenic purpura,” was published in the journal Blood Research.
Thrombotic microangiopathies (TMA) are a group of conditions characterized by the abnormal formation of blood clots in small blood vessels, leading to the destruction of red blood cells (hemolytic anemia) and organ damage.
Two such conditions are atypical hemolytic uremic syndrome (aHUS) and thrombotic thrombocytopenic purpura (TTP). However, despite the similar features of these conditions, they have very different causes.
aHUS is caused by the uncontrolled activation of the complement system — the part of the immune system made up of several blood proteins that enhances (complements) an immune response — leading to the formation of blood clots.
In contrast, TTP is caused by a deficiency in an enzyme involved in blood clotting, known as ADAMTS13 (a disintegrin and metalloproteinase with thrombospondin type 1 motif, member 13).
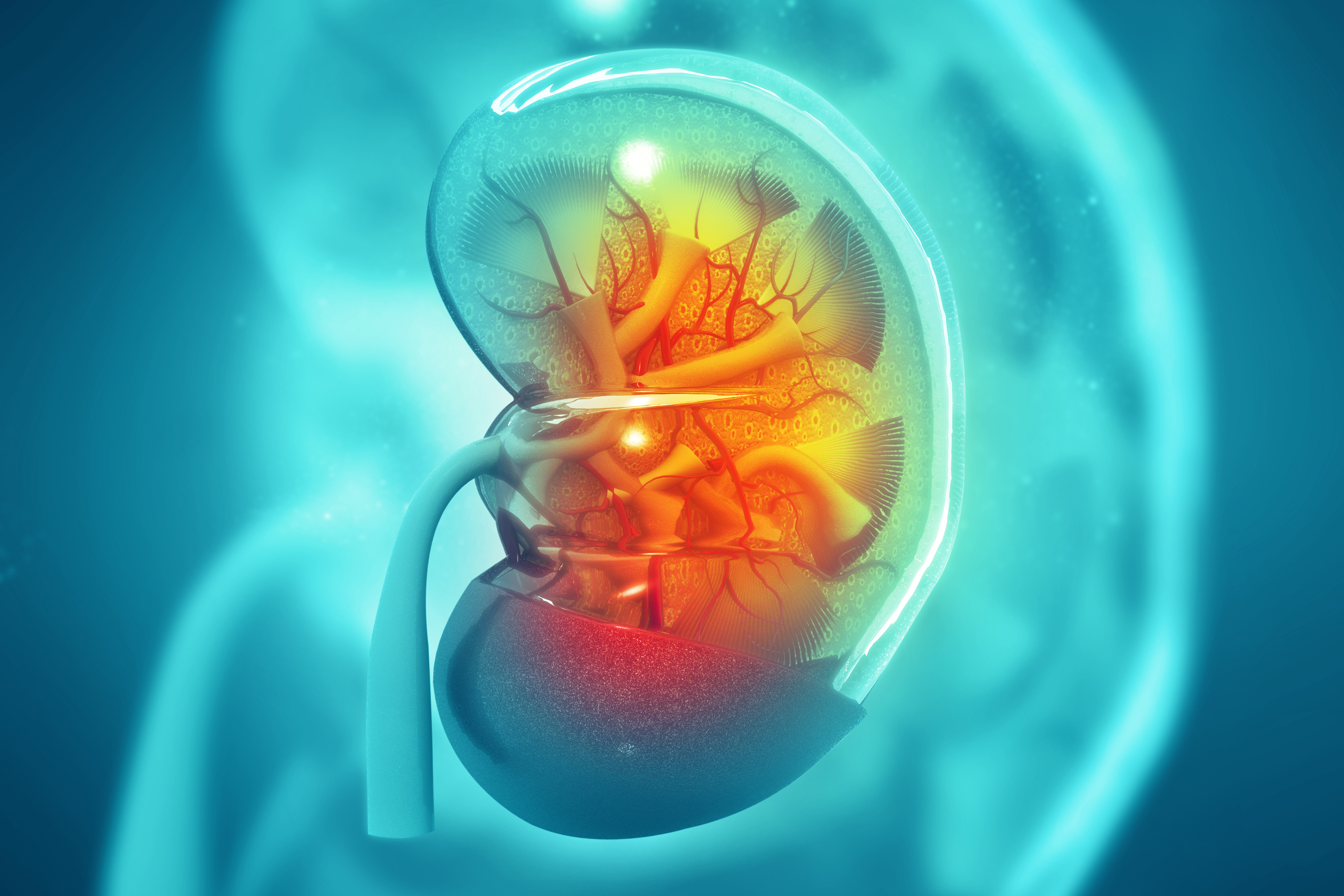
Although the symptoms of the two conditions overlap, aHUS shows more severe renal (kidney) involvement, while TPP predominantly presents neurological symptoms.
Due to the sharing of clinical manifestations, it can be difficult to distinguish these conditions in the clinic. That is why it is important to identify reliable markers to help differentiate them and more accurately predict patient prognosis.
To this end, a team of researchers based at the CHA University in Korea analyzed the records of 48 TTP patients, as identified by an ADAMTS13 deficiency, and 50 aHUS patients, 18 years and older, who did not have an ADAMTS13 deficiency.
Their goal was to determine whether markers from complement activation and ADAMTS13 activity could be used to differentiate aHUS from TTP.
In addition, the information was analyzed to better predict the response to a therapy used to treat patients with a low blood platelet count — a hallmark of both aHUS and TTP. The therapy, known as plasma exchange therapy (PEX or PET), increases the numbers of platelets by mixing a patient’s blood cells with fresh plasma.
The team examined the clinical information and blood samples collected at admission from aHUS and TTP patients who were newly diagnosed, as well as 40 healthy control samples — focusing on markers of complement activation and ADAMTS13 activity — to identify any relationship with aHUS patient outcomes.
Data regarding the PEX treatments and prognoses were obtained six months after blood samples were collected.
The analysis showed that markers for complement activation were significantly higher in people with aHUS compared to the healthy controls.
However, the levels of these markers between the aHUS and TTP patients were not significantly different, with the exception of a single marker (factor Bb) that was higher in aHUS patients. Additionally, markers for abnormal complement activation were not linked to poorer outcomes in aHUS or TTP patients.
Interestingly, assessment of ADAMTS13 activity revealed that, while TTP patients had abnormally low levels of activity as expected, in 50% of aHUS patients, high ADAMTS13 activity was found.
The higher-than-normal ADAMTS13 activity was related significantly to better outcomes such as improved response to PEX treatment and stabilized platelet counts (remission), plus a reduction in the rate of exacerbation and mortality. The recurrence (relapse) of aHUS or TTP after remission was not related to ADAMTS13 activity.
“[T]he results of our study suggest that ADAMTS13 activity can be used to determine the appropriate treatment options for aHUS patients as a result of differentiation from TTP patients, in addition to serving as a prognostic indicator to determine whether additional therapies, such as Eculizumab [Soliris], should be administered,” the researchers stated.
Statistical analysis found that the best predictors for better aHUS treatment outcomes were high levels of ADAMTS13 activity, normal levels of serum creatinine (high levels indicate acute kidney damage), and a stabilized platelet count.
In TTP patients, none of the factors were determined to be linked to better outcomes.
According to the study authors, “this is the first report linking high normal ADAMTS13 activity with improved outcomes of PEX treatments in aHUS patients.”
“These measures may distinguish patients requiring more intensive management, and the results presented here lay the groundwork for future multicenter studies aimed at identifying prognostic markers for aHUS and TMA,” they concluded.